Recommended Global Nursing Webinars & Conferences
Asia Pacific & Middle East
Nurse Education 2026
- Welcome Message
- About Conference
- Sessions and Tracks
- Market Analysis Report
- Important Guidelines and Deadlines
- Past Conference Report
Welcome Message
It is with great pleasure that we welcome you to the 5th World Congress on Nursing Education & Management, taking place on January 26–27, 2026, in the vibrant city of Barcelona, Spain. This prestigious gathering will bring together nursing professionals, educators, researchers, and healthcare leaders from around the globe to share knowledge, exchange ideas, and explore innovative approaches in nursing education, clinical practice, and healthcare management.
Over the course of two enriching days, participants will have the opportunity to engage in thought-provoking discussions, attend insightful keynote sessions, and network with peers who are shaping the future of nursing. Barcelona, with its rich cultural heritage and warm hospitality, provides the perfect backdrop for this collaborative exchange of ideas and experiences.
We look forward to your active participation in making this congress a memorable and impactful event for the global nursing community.
See you in Barcelona!
About Conference
The 5th World Congress on Nursing Education & Management will be held on January 26–27, 2026, in Barcelona, Spain, bringing together nursing professionals, educators, administrators, researchers, and healthcare innovators from across the globe. This premier international event serves as a platform to share the latest advancements, evidence-based practices, and emerging trends in nursing education, clinical care, and healthcare leadership.
The congress will feature a dynamic program of keynote presentations, interactive panel discussions, hands-on workshops, and poster sessions, offering valuable opportunities for professional development and knowledge exchange. Participants will explore topics such as innovative teaching methodologies, nursing leadership strategies, healthcare policy, patient-centered care, digital transformation in nursing, and the role of management in enhancing healthcare outcomes.
By fostering global collaboration and interdisciplinary learning, this congress aims to inspire excellence in nursing practice, empower future leaders, and promote advancements in healthcare delivery worldwide. Delegates will also enjoy the cultural richness and charm of Barcelona, making this both an academic and memorable experience.
Join us in shaping the future of nursing education and management at this landmark gathering.
Who Can Attend?
The 5th World Congress on Nursing Education & Management welcomes professionals, researchers, educators, policymakers, and students from all areas of nursing and healthcare. This includes specialists in cancer, cardiac, critical care, adult and women’s health, legal nursing, pediatric and emergency nursing, midwifery, public health, and healthcare management. Participants from clinical practice, research, administration, policy-making, and academia will come together on this platform to exchange ideas, share expertise, and develop collaborative solutions aimed at achieving optimal health outcomes.
Why Attend?
This global gathering provides a unique opportunity to engage with the latest developments in nursing education, clinical practice, and healthcare leadership. Attendees can gain valuable insights into innovative care models, educational methodologies, and management strategies from leading experts worldwide. For students, the congress offers exposure to the forefront of the nursing profession, fostering connections within the scientific and healthcare communities that can be invaluable for career growth. Whether you are an experienced professional or an aspiring nurse, this event is designed to broaden perspectives, inspire innovation, and strengthen the global nursing network.
Sessions and Tracks
Track 01. Curriculum Development
Curriculum development in nursing education is a foundational process that ensures the preparation of competent, ethical, and adaptable nursing professionals. It involves continuous assessment and redesign to align with evolving healthcare demands, technological advancements, and global health trends. A modern nursing curriculum emphasizes competency-based learning, integrating theory with practical application and fostering critical thinking, cultural sensitivity, and clinical reasoning. It prepares students not just to perform tasks, but to understand the broader implications of their care within diverse and dynamic healthcare systems. Collaboration among educators, clinical partners, accreditation bodies, and healthcare stakeholders is essential in shaping a curriculum that reflects real-world needs. Incorporating interdisciplinary topics, evidence-based practices, and global health issues helps future nurses become well-rounded professionals. Moreover, faculty must be equipped with the knowledge and skills to design and deliver updated content using innovative methodologies. Curriculum development is not a one-time effort but a strategic, evolving process that directly influences patient outcomes and the quality of care. By continually revisiting and refining the educational framework, nursing institutions ensure their graduates are well-prepared to face complex clinical environments and lead transformative changes in healthcare.
Track 02. Simulation Learning
Simulation learning has emerged as a powerful educational tool in nursing, bridging the gap between classroom theory and clinical practice by offering students a safe, realistic environment to develop hands-on skills. Through the use of high-fidelity mannequins, virtual simulations, and standardized patients, learners can engage in lifelike scenarios that mirror complex clinical conditions, emergencies, and interpersonal interactions. This approach enhances critical thinking, decision-making, and communication abilities while boosting student confidence and reducing anxiety prior to real-world patient care. One of the most valuable components of simulation is the debriefing process, where students reflect on their performance, receive feedback, and internalize lessons learned. It also provides a platform for interprofessional collaboration, preparing nursing students to work efficiently within diverse healthcare teams. Simulation learning contributes significantly to patient safety by allowing students to make and correct errors without risk. With the integration of new technologies like augmented reality and artificial intelligence, simulation is becoming even more immersive and effective. Its role in nursing education is vital, offering a dynamic and engaging path for students to master clinical competencies and prepare for high-pressure healthcare settings.
Track 03. Nursing Leadership
Nursing leadership is a critical element in the delivery of high-quality healthcare, encompassing the ability to guide teams, advocate for patients, manage resources, and drive organizational improvement. It extends beyond traditional administrative roles to include any nurse who influences practice and inspires positive change. Effective nurse leaders possess strong communication, emotional intelligence, ethical reasoning, and strategic thinking skills, which are essential in navigating complex clinical environments. Leadership development begins in nursing education through structured training, mentorship programs, and exposure to real-world healthcare challenges. As the healthcare landscape becomes more interdisciplinary and patient-centered, the demand for nurses who can lead with vision, empathy, and resilience continues to grow. Nurse leaders play a key role in shaping policy, enhancing team dynamics, promoting evidence-based practices, and ensuring that care delivery meets the highest standards. In times of crisis, such as pandemics or systemic reforms, their ability to coordinate care, manage uncertainty, and support their teams is especially vital. Investing in leadership education empowers nurses to become proactive change agents, ultimately elevating the entire profession and improving health outcomes across systems.
Track 04. Faculty Development
Faculty development in nursing education plays a pivotal role in maintaining the quality and relevance of academic programs by empowering educators with the skills and knowledge needed to excel in teaching, leadership, research, and mentorship. As healthcare and education continue to evolve, faculty must adapt to new technologies, pedagogical strategies, and regulatory expectations. Development initiatives include training in innovative teaching methodologies such as simulation, digital learning platforms, active learning strategies, and assessment techniques. These programs also promote scholarly activity, leadership growth, and interprofessional collaboration, ensuring that faculty remain engaged and informed contributors to both academia and clinical practice. Continuous faculty development fosters a culture of excellence, where educators can reflect on their practices, stay updated with evidence-based education trends, and effectively mentor students. It also supports institutional goals by promoting curriculum quality, accreditation standards, and research productivity. When faculty members are well-prepared and supported, they inspire students, elevate the learning environment, and contribute significantly to producing competent, compassionate, and future-ready nursing professionals.
Track 05. Digital Pedagogy
Digital pedagogy in nursing education refers to the strategic use of technology to enhance teaching and learning experiences, fostering a more interactive, flexible, and accessible environment for students. As digital tools become integral to healthcare, nursing educators are incorporating online learning platforms, virtual classrooms, interactive simulations, and multimedia content to support diverse learning styles and bridge geographical barriers. This shift enables the integration of real-time assessments, immediate feedback, and self-paced modules that support individualized learning journeys. Digital pedagogy also encourages collaborative learning through discussion forums, peer reviews, and group projects hosted in virtual spaces. Educators must be adept at selecting appropriate technologies, designing inclusive and engaging content, and ensuring digital literacy among students. Furthermore, ethical considerations such as data privacy, accessibility, and digital professionalism are vital components of this approach. As the healthcare industry increasingly relies on digital competencies, incorporating digital pedagogy into nursing education ensures that future professionals are not only clinically proficient but also technologically fluent. This transformation enhances educational quality, supports lifelong learning, and prepares nurses to operate effectively in an evolving, tech-driven healthcare system.
Track 06. Student Assessment
Student assessment is a fundamental component of nursing education that evaluates learners’ knowledge, skills, clinical judgment, and professional behavior throughout their academic journey. Effective assessment strategies provide valuable insights into student progress, guide instructional improvements, and ensure that graduates meet required competencies for safe and ethical practice. Traditional exams, while still relevant, are increasingly complemented by formative assessments such as reflective journals, clinical simulations, peer assessments, and portfolio reviews. Objective Structured Clinical Examinations (OSCEs) have become widely used for assessing hands-on skills and decision-making under pressure. Digital tools also enable real-time quizzes, interactive case studies, and data-driven evaluations, making assessment more dynamic and responsive. Continuous, multifaceted evaluation methods help identify areas of improvement early and provide students with the feedback needed to self-correct and grow. Importantly, assessment must be transparent, fair, and aligned with clearly defined learning outcomes. When implemented effectively, student assessment not only certifies academic achievement but also promotes critical thinking, accountability, and readiness for real-world clinical environments.
Track 07. Interdisciplinary Education
Interdisciplinary education is increasingly essential in nursing programs as healthcare systems move toward team-based, collaborative care models. This educational approach brings together students from different health professions—such as medicine, pharmacy, social work, and physiotherapy—to learn with, from, and about each other. The goal is to foster mutual respect, improve communication, and enhance understanding of each discipline’s role in patient care. Through interdisciplinary education, nursing students develop the competencies required for effective teamwork, shared decision-making, and holistic patient management. Simulation exercises, collaborative case studies, joint clinical rotations, and interdisciplinary seminars are among the strategies used to promote this collaborative learning. As healthcare becomes more complex, the ability to function within diverse teams directly impacts patient safety, satisfaction, and outcomes. For nursing students, exposure to interdisciplinary education builds confidence, leadership, and a systems-thinking mindset. It ultimately prepares them to contribute effectively within integrated care teams that are essential for managing chronic diseases, coordinating transitions of care, and addressing social determinants of health.
Track 08. Clinical Supervision
Clinical supervision is a vital process in nursing education that provides students with structured guidance, feedback, and support during their clinical training. It ensures that learners apply theoretical knowledge to real-life practice while developing essential competencies such as patient care, communication, time management, and ethical decision-making. Supervision is typically carried out by experienced nurses, educators, or preceptors who mentor students, model professional behaviors, and evaluate performance in real-time. Effective clinical supervision fosters reflective practice, encourages continuous improvement, and builds student confidence in handling complex situations. It also plays a critical role in maintaining patient safety by ensuring that students receive appropriate oversight as they gain hands-on experience. A successful supervision model balances challenge with support, allowing students to grow while minimizing the risk of burnout or anxiety. With the increasing demands of clinical settings, supervision must also evolve to include tools like digital documentation, mobile assessments, and remote check-ins to enhance accessibility and consistency. Ultimately, clinical supervision is key to bridging the academic-practice gap and shaping competent, compassionate, and practice-ready nursing professionals.
Track 09. Evidence-Based Teaching
Evidence-based teaching in nursing education is a pedagogical approach that integrates the best available research, educational theory, and clinical expertise to guide instructional decisions and improve learning outcomes. This method ensures that teaching strategies are not only innovative but also scientifically validated to support student engagement, knowledge retention, and skill development. Educators who embrace evidence-based teaching continuously evaluate the effectiveness of their methods through student feedback, performance data, and academic research. Techniques such as active learning, flipped classrooms, problem-based scenarios, and simulation-based exercises are commonly used, as they have been shown to foster critical thinking, deeper understanding, and real-world application. By modeling evidence-based practices in the classroom, faculty also instill a mindset of inquiry and continual learning in students, preparing them to seek out and apply the latest clinical evidence in their future practice. Furthermore, this approach strengthens the bridge between education and healthcare delivery, ensuring that nursing graduates are equipped with not only practical skills but also the ability to question, analyze, and improve care through evidence.
Track 10. Change Management
Change management in nursing education and practice involves guiding individuals and organizations through transitions brought on by new technologies, evolving healthcare policies, curriculum reforms, or shifts in patient care models. With healthcare environments becoming increasingly complex and dynamic, the ability to adapt to change is a critical competency for both educators and practitioners. In academic settings, change management might include implementing new learning technologies, revising curricula, or shifting toward competency-based education. In clinical practice, it involves embracing innovations in care delivery, interdisciplinary collaboration, and patient-centered approaches. Successful change management requires effective leadership, clear communication, stakeholder engagement, and an understanding of organizational culture. Educators must teach students not only how to adapt to change but also how to lead it—fostering resilience, flexibility, and proactive thinking. Integrating principles of change theory and project management into nursing programs helps prepare future nurses to navigate and influence change with confidence. Ultimately, managing change effectively leads to improved educational practices, stronger healthcare systems, and better patient outcomes.
Track 11. Workforce Retention
Workforce retention in nursing is a pressing concern that directly impacts healthcare quality, patient safety, and the long-term sustainability of healthcare systems. High turnover rates lead to staffing shortages, increased workloads, burnout, and diminished morale among remaining staff. In nursing education, addressing retention begins with preparing students for the realities of clinical practice while equipping them with coping mechanisms, self-care strategies, and a strong professional identity. Educational programs that emphasize mentorship, leadership, emotional intelligence, and career development contribute to long-term job satisfaction and career commitment. On an organizational level, strategies for retention include fostering supportive work environments, offering competitive compensation, recognizing achievements, and providing continuous learning opportunities. Creating a culture of respect, inclusivity, and teamwork also plays a crucial role in employee satisfaction and retention. Faculty and nurse leaders must work together to build a resilient, empowered workforce capable of withstanding the challenges of modern healthcare. A focus on workforce retention ensures not only the well-being of nurses but also the continuity of quality care across all healthcare settings.
Track 12. Patient Safety
Patient safety is a core pillar of nursing education and practice, emphasizing the prevention of errors, the reduction of harm, and the delivery of high-quality, evidence-based care. From the very beginning of their education, nursing students must be trained to prioritize safety in all aspects of clinical care, including medication administration, infection control, communication, documentation, and decision-making. Simulation-based learning, root cause analysis exercises, and clinical case discussions are key strategies used to embed safety principles into education. Faculty play a crucial role in modeling safe practices and fostering a culture of accountability and continuous improvement. Effective patient safety education also includes interprofessional training, where nurses collaborate with other healthcare professionals to improve coordination and reduce risks. With the healthcare landscape growing more complex, nurses must also be equipped to identify system-level issues, report near-misses, and advocate for policy changes that enhance safety. A strong foundation in patient safety leads to better outcomes, reduced healthcare costs, and greater trust between patients and healthcare providers. Teaching safety as a fundamental value empowers nursing students to become vigilant, competent, and ethical practitioners.
Track 13. Resource Allocation
Resource allocation in nursing education and practice involves the effective distribution of available resources—human, financial, technological, and material—to ensure quality care and optimal learning outcomes. In academic settings, this includes budgeting for faculty development, simulation labs, student support services, and up-to-date learning technologies. In clinical practice, it pertains to managing staff workloads, equipment, supplies, and time in a way that promotes patient safety and staff well-being. For nurse managers and educators, understanding the principles of resource allocation is essential to making informed decisions in environments where resources are often limited and demands are high. Ethical considerations are also critical, as equitable access to resources must be ensured for both students and patients. Nursing students must be taught how to prioritize needs, assess risks, and advocate for efficient use of resources within multidisciplinary teams. Integrating resource management skills into the nursing curriculum prepares future nurses to contribute to cost-effective, evidence-based practices without compromising quality. Effective resource allocation supports sustainability in healthcare and education, promotes staff retention, and improves overall system performance.
Track 14. Quality Improvement
Quality improvement (QI) in nursing is a continuous, systematic process aimed at enhancing patient outcomes, improving work processes, and fostering a culture of excellence within healthcare and academic institutions. In nursing education, students are taught the principles of QI through case studies, project-based learning, and clinical practicums where they identify gaps in care or instruction and propose evidence-based solutions. QI involves the use of tools such as the Plan-Do-Study-Act (PDSA) cycle, root cause analysis, and performance metrics to assess and enhance healthcare delivery or educational practices. Faculty and clinical mentors play a vital role in instilling a QI mindset, encouraging curiosity, innovation, and accountability. Teaching QI equips nursing students with the skills to measure the effectiveness of interventions, collaborate across disciplines, and lead change initiatives. In clinical environments, QI projects have been instrumental in reducing medication errors, lowering infection rates, and improving patient satisfaction. By embedding QI into nursing education, institutions prepare future nurses not just to follow protocols but to actively evaluate and improve them—driving progress in patient care and professional standards.
Track 15. Ethical Administration
Ethical administration in nursing refers to the leadership and management practices guided by integrity, fairness, accountability, and respect for human dignity in both educational and clinical environments. Nurse administrators often face complex decisions involving staff management, patient care, policy enforcement, and resource distribution—all of which carry ethical implications. In academic settings, ethical administration encompasses equitable grading, academic honesty, inclusive teaching practices, and fair faculty-student relationships. In clinical contexts, administrators must ensure ethical hiring, confidentiality, safe working conditions, and compliance with healthcare laws and ethical codes. Nursing education must therefore include training in ethical decision-making, professional codes of conduct, and organizational ethics to prepare future leaders for the challenges of modern healthcare. Ethical administration promotes transparency, trust, and equity—fostering environments where both patients and professionals feel valued and protected. When administrators lead with ethics at the core of their practices, they inspire a culture of accountability and compassion that enhances the quality and integrity of both education and care delivery.
Track 16. Care Coordination
Care coordination is a vital component of modern nursing that involves organizing patient care activities and information sharing across multidisciplinary teams to ensure timely, efficient, and person-centered healthcare delivery. In today’s fragmented healthcare systems, care coordination helps reduce redundancies, prevent errors, and improve transitions between providers and settings—especially for patients with chronic conditions or complex needs. Nursing students must be trained in communication, teamwork, documentation, and systems thinking to effectively manage care pathways and advocate for their patients. Education on care coordination often includes simulation exercises, case management scenarios, and interprofessional collaboration modules. Nurses serve as the bridge between patients, families, physicians, social workers, and other care professionals, ensuring that care plans are understood and followed. Faculty also emphasize the importance of cultural competence, health literacy, and shared decision-making in achieving effective coordination. Through proactive care coordination, nurses contribute to better health outcomes, increased patient satisfaction, and lower healthcare costs. By integrating this concept into nursing curricula, educators empower students to take on a leadership role in delivering holistic, organized, and responsive care.
Track 17. Mental Health Nursing
Mental health nursing is a specialized field that focuses on the care and support of individuals experiencing psychological distress, psychiatric disorders, or emotional challenges. With the global rise in mental health issues, it has become essential for nursing education to provide students with a deep understanding of mental health concepts, therapeutic communication, crisis intervention, and stigma reduction. Mental health nurses play a key role in assessment, diagnosis, treatment, and recovery support, often working within multidisciplinary teams in hospitals, clinics, and community settings. Nursing curricula must include exposure to psychiatric nursing theories, evidence-based treatment approaches, and practical training through simulation or clinical placements in mental health facilities. Equally important is cultivating empathy, cultural competence, and non-judgmental care attitudes among students. Educators should emphasize early identification of symptoms, suicide prevention strategies, trauma-informed care, and the integration of mental health in primary care. As mental well-being becomes a central aspect of holistic patient care, preparing nurses with specialized knowledge and compassionate skills in mental health nursing is crucial for improving quality of life, reducing relapses, and promoting recovery for individuals and families affected by mental illness.
Track 18. Professional Advancement
Professional advancement in nursing refers to the continuous growth and development of nurses throughout their careers, supported by education, mentorship, certification, and leadership opportunities. It begins during academic preparation, where students are introduced to career planning, role development, and specialization paths that align with personal goals and healthcare needs. Opportunities for advancement include pursuing higher degrees, gaining clinical specializations, participating in research, taking on administrative roles, and engaging in policy advocacy. Educators play a vital role in encouraging ambition, guiding academic pathways, and instilling lifelong learning habits. Structured mentorship programs, leadership training, and exposure to healthcare innovations help nurses build the confidence and skills needed to advance professionally. Furthermore, institutions must foster environments that recognize and reward professional growth through promotions, continuing education support, and access to leadership roles. Emphasizing professional advancement in nursing education not only enhances individual career trajectories but also strengthens healthcare systems by ensuring that nurses are equipped to take on complex responsibilities, innovate practice, and lead the future of nursing.
Track 19. Policy Implementation
Policy implementation in nursing involves the translation of healthcare policies into daily practice, influencing how care is delivered, managed, and evaluated within various clinical and academic settings. Nurses play a crucial role in this process by ensuring that policies are applied accurately, ethically, and in alignment with patient needs and organizational goals. In nursing education, students must learn how health policies are formulated, interpreted, and enacted, particularly in areas like patient safety, infection control, staffing regulations, and quality standards. Educators can incorporate real-world policy scenarios, role-playing, and health systems analysis to teach these concepts. Nurses also serve as advocates and change agents, contributing to the development of policies that address disparities, promote health equity, and support patient-centered care. By understanding policy structures and implementation processes, nurses are better prepared to comply with regulations, engage in quality improvement initiatives, and participate in institutional decision-making. Empowering nursing students with policy knowledge enables them to influence healthcare reform and ensure that policies are implemented with compassion, evidence, and professional insight.
Track 20. Performance Measurement
Performance measurement in nursing is the systematic evaluation of individual, team, and organizational effectiveness using predefined standards and indicators. It plays a central role in maintaining accountability, improving care quality, and informing strategic decisions in both clinical practice and nursing education. Metrics such as patient outcomes, satisfaction scores, medication error rates, hand hygiene compliance, and documentation accuracy are commonly used in healthcare settings to assess nursing performance. In educational environments, student performance is measured through academic assessments, clinical evaluations, and professional behavior benchmarks. Teaching students the principles of performance measurement enables them to understand how their actions directly impact patient safety and institutional efficiency. Faculty can integrate performance dashboards, data analysis exercises, and feedback loops to help learners develop a results-driven mindset. Nurses involved in leadership and management must also be adept at interpreting performance data to identify trends, allocate resources, and guide policy changes. A culture of continuous performance measurement fosters excellence, transparency, and accountability—qualities that are essential for advancing the nursing profession and improving healthcare delivery systems.
Track 21. Artificial Intelligence in Nursing
Artificial intelligence in nursing is rapidly reshaping the healthcare environment by enhancing clinical efficiency, streamlining administrative processes, and supporting evidence-based patient care. From automating routine documentation to providing diagnostic assistance, AI empowers nurses to focus more on direct patient interaction and complex clinical judgments. Natural language processing tools can transcribe and organize nursing notes in real time, while AI-driven decision systems suggest optimal care plans based on patient histories and evidence-based guidelines. These technologies also enhance communication and coordination within multidisciplinary teams by predicting patient care needs and flagging potential safety issues. For nurse managers and educators, AI offers powerful analytics to evaluate performance metrics, predict staffing requirements, and personalize educational content. While its benefits are transformative, the adoption of AI in nursing also demands a solid understanding of digital ethics, data privacy, and critical appraisal of machine-generated insights. Training programs must now evolve to equip nurses with the competencies required to collaborate with intelligent systems and maintain the human-centered approach central to nursing. As artificial intelligence becomes more deeply embedded into healthcare systems, nurses will increasingly act as interpreters of AI insights, ensuring that technology complements rather than replaces clinical empathy and judgment. The integration of AI in nursing represents not just a technological shift, but a profound evolution in the way compassionate care is delivered and supported in a data-rich environment.
Track 22. Smart Simulation Tools
Smart simulation tools are revolutionizing nursing education by offering realistic, data-driven environments where learners can safely develop and refine their clinical skills. These tools combine artificial intelligence, virtual reality, and advanced analytics to create interactive scenarios that respond dynamically to student decisions, mirroring real-life clinical outcomes. Unlike traditional simulations, smart systems can assess the learner’s responses in real time and provide immediate, personalized feedback that enhances critical thinking and decision-making abilities. Virtual patients, equipped with lifelike physiological reactions and voice-enabled interactions, help students practice assessment, communication, and interventions in complex care situations — from emergency response to chronic illness management. Educators benefit from automated performance tracking, which allows for objective evaluation and tailoring of content to meet individual learning needs. Additionally, smart simulation supports interprofessional education by enabling collaboration among students from different healthcare disciplines within a shared virtual space. This fosters teamwork and coordination skills essential for real-world practice. The adaptability of these tools makes them ideal for both in-person and remote learning environments, expanding access to high-quality education across geographical boundaries. Importantly, smart simulation helps bridge the gap between theoretical knowledge and hands-on practice, reducing anxiety among novice nurses and improving clinical readiness. As the demand for skilled, confident nursing professionals grows, the adoption of smart simulation tools ensures that learners are not only competent but also prepared to deliver safe, patient-centered care in a rapidly evolving healthcare landscape.
Track 23. Machine Learning in Education
Machine learning is transforming the landscape of nursing education by enabling personalized learning experiences, automating assessments, and enhancing curriculum design through data-driven insights. By analyzing patterns in student performance and behavior, machine learning algorithms can identify individual learning needs and adapt educational content accordingly, ensuring that each student receives targeted support to overcome their challenges and build on their strengths. This level of personalization promotes greater student engagement, improved knowledge retention, and higher academic success rates. Machine learning also streamlines administrative tasks by grading assignments, tracking attendance, and predicting student outcomes, thereby allowing educators to focus more on interactive teaching and mentoring. In curriculum development, machine learning tools can analyze vast educational datasets to identify content gaps, optimize course structure, and align learning objectives with evolving clinical competencies. Moreover, in simulation-based learning, machine learning enhances realism by modeling dynamic patient responses and adjusting scenarios based on learner actions, fostering critical thinking and decision-making skills. The technology also contributes to evaluating the effectiveness of teaching strategies by generating real-time feedback and performance analytics, which educators can use to refine their methods. As machine learning continues to evolve, it will likely play an increasingly central role in creating more efficient, responsive, and student-centered nursing education systems. Embracing this technology ensures that nursing graduates are not only academically prepared but also equipped with the digital literacy needed to thrive in modern healthcare environments.
Track 24. Virtual Nursing Assistants
Virtual nursing assistants are emerging as a transformative tool in both nursing education and clinical practice, offering real-time support, guidance, and information through artificial intelligence-powered interfaces. In educational settings, these digital assistants serve as interactive learning aids, capable of answering student queries, reinforcing theoretical concepts, and simulating patient interactions. By offering 24/7 access to reliable, consistent information, virtual nursing assistants help bridge the gap between classroom instruction and clinical practice, supporting self-paced learning and encouraging greater autonomy among students. These tools can be programmed to simulate patient care scenarios, guide students through evidence-based procedures, and provide immediate feedback on their decisions, helping to reinforce critical thinking and clinical judgment. In healthcare management, virtual assistants play a key role in supporting nurses with routine administrative and clinical tasks, such as patient scheduling, medication reminders, symptom triage, and data documentation. This reduces the cognitive load on nursing staff, allowing them to devote more time to direct patient care and decision-making. As the healthcare industry increasingly adopts digital solutions, integrating virtual nursing assistants into nursing curricula also ensures that students develop the competencies required to interact with and manage these tools effectively. Additionally, these systems can be integrated with electronic health records, enhancing workflow efficiency and improving communication across multidisciplinary teams. By familiarizing students with virtual nursing assistants early in their education, institutions prepare future nurses to work efficiently in technologically advanced environments, ultimately improving patient safety, satisfaction, and care outcomes.
Market Analysis Report
The global nursing education and management sector is experiencing steady growth, driven by the worldwide nursing shortage, rising healthcare demands, and rapid expansion of training infrastructure. The nursing education market was valued at approximately USD 8.8 billion in 2023, with North America holding a major share due to high healthcare expenditure and advanced training facilities. Institutions are increasingly adopting hybrid learning models, simulation-based training, and competency-focused curricula to address both clinical and leadership skills. Workforce retention has become a critical management priority, with healthcare organizations investing in leadership programs, flexible staffing models, and strategies to improve nurse well-being.
The market is projected to grow at an estimated 4–5% compound annual growth rate for core nursing education, with related segments like healthcare simulation expected to expand at over 15% annually. Persistent shortages—estimated at 4.5 million nurses globally by 2030—are driving demand for expanded education capacity and advanced management capabilities. Digital transformation is playing a key role, with virtual reality, artificial intelligence–driven adaptive learning, and remote simulation making training more scalable and accessible. Policy initiatives and accreditation requirements are increasingly emphasizing leadership training, interprofessional collaboration, and quality outcomes.
Challenges include faculty shortages that limit student intake capacity, disparities in training resources between high- and low-income countries, and variations in standards that hinder workforce mobility. Addressing these issues through affordable digital solutions, educator training, and global collaboration will be essential. With sustained investment and innovation, nursing education and management will continue to be a critical driver of healthcare system resilience and the delivery of high-quality patient care worldwide.
International Associations and Societies:
- International Council of Nurses (ICN)
- Sigma Theta Tau International Honor Society of Nursing
- National League for Nursing (NLN)
- American Organization for Nursing Leadership (AONL)
- International Network for Doctoral Education in Nursing (INDEN)
- Canadian Association of Schools of Nursing (CASN)
- European Federation of Nurses Associations (EFN)
- Commonwealth Nurses and Midwives Federation (CNMF)
- International Society for Professional Identity in Nursing (ISPIN)
- World Health Organization – Nursing and Midwifery
- Learn the latest in nursing education and leadership.
- Gain skills through interactive workshops and sessions.
- Network with global nursing professionals and decision makers.
- Present and share your research or projects with feedback.
- Receive DOI assignment for accepted abstracts/papers (enhances visibility and citation).
- Earn a certificate of participation or continuing education credit.
- Access keynote and expert panel insights.
- Complimentary breakfast and refreshment breaks.
- Opportunity for publication in conference proceedings or affiliated journals.
- Meet potential collaborators, mentors, and employers.
- Receive conference materials and resource kits.
- Priority access to recorded sessions or digital content.
- Recognition through awards or highlighted presentations.
- Enhanced resume/CV profile with international engagement.
- Cultural and destination experience in Barcelona.
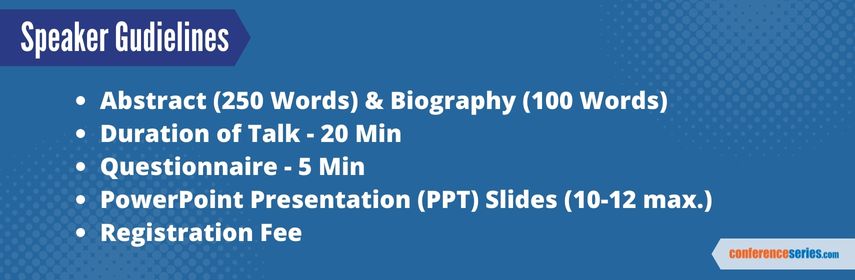
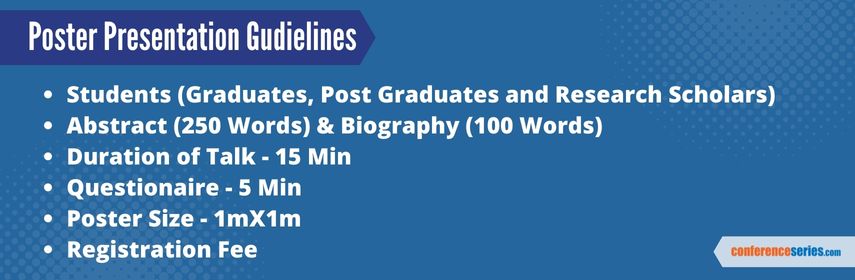
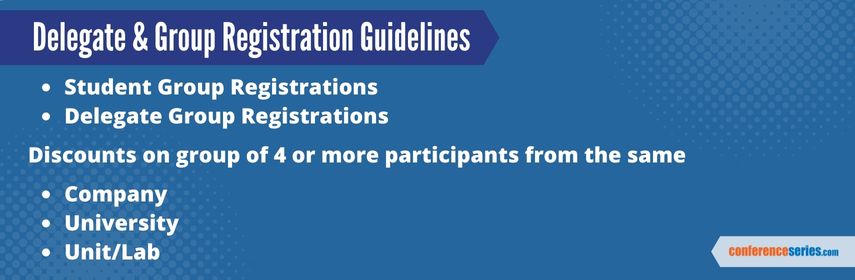
Important Guidelines and Deadlines
We are pleased to invite researchers, educators, and healthcare professionals to submit their abstracts for the 5th World Congress on Nursing Education & Management, scheduled to take place on January 26–27, 2025, in Barcelona, Spain.
Abstract Submission is Now Open!
Submit your abstract now and become a part of this global platform to advance nursing education, leadership, and innovation. All abstracts will undergo a peer-review process, and selected authors will be invited for oral or poster presentations during the conference.
-
Last Date for Abstract Submission: January 20, 2025
-
Notification of Acceptance: Within 7 days of submission
-
Registration Opens: August 05, 2025
-
Early Bird Registration Closes: September 26, 2025
-
Final Registration Deadline: January 20, 2025
Guidelines for Abstract Submission:
-
Abstracts should be submitted in English.
-
Word limit: 250–300 words.
-
Include title, author(s) name, affiliation, and contact details.
-
Topics must align with nursing education, clinical practice, management, or innovation.
-
Upload via our official submission portal or email to: [email protected]
Need Help?
If you require assistance or an official invitation letter for visa or institutional approval, please contact our organizing committee at [email protected].
We look forward to receiving your contributions and welcoming you to Barcelona in January 2025!
Past Conference Report
Nurse Education 2023
Nursing Conferences extends its welcome to 4th World Congress on Nursing Education & Management, on November 29-30, 2023 at Kualalumpur, Malaysia. With a theme “Future Enhancement and Best Practices in Nursing Care”
Nursing Conferences Organizes 1000+ Conferences Every Year across USA, Europe & Asia with support from 1000 more scientific societies and Publishes 700+ Open access journals which contains over 100000 eminent personalities, reputed scientists as editorial board members.
In support of improving patient care, this Nursing Education Conference has been planned and implemented by Conference Series, Ltd and Center for Education Development (CED). CED is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Past Reports Gallery
To Collaborate Scientific Professionals around the World
Conference Date January 26-27, 2026
For Sponsors & Exhibitors
Speaker Opportunity
Useful Links
Supported By
All accepted abstracts will be published in respective Conference Series International Journals.
Abstracts will be provided with Digital Object Identifier by